Overview
The article defines a clinical study monitor as a pivotal figure in the oversight of clinical trials, tasked with ensuring compliance with regulatory standards and safeguarding participant welfare through essential activities such as site visits and data review. This role has evolved significantly, reflecting an increase in responsibilities that correspond to the growing complexity of clinical research.
Consequently, the monitor's importance in maintaining data integrity and participant safety is underscored, particularly with the integration of advanced technologies like AI and remote monitoring tools. This evolution not only highlights the monitor's critical function but also emphasizes the need for ongoing adaptation to new challenges in the field.
Introduction
A clinical study monitor, often referred to as a Research Associate, serves as a cornerstone of clinical research, ensuring adherence to regulatory standards and ethical guidelines. This role has evolved significantly, expanding from basic compliance checks to a multifaceted position that encompasses risk management, data integrity, and participant safety.
As the complexity of clinical trials increases, these monitors encounter numerous challenges in maintaining quality and compliance. Furthermore, emerging technologies are reshaping their responsibilities, prompting a reevaluation of their functions.
This exploration delves into the vital roles of clinical study monitors and underscores the critical importance of their work in advancing medical research.
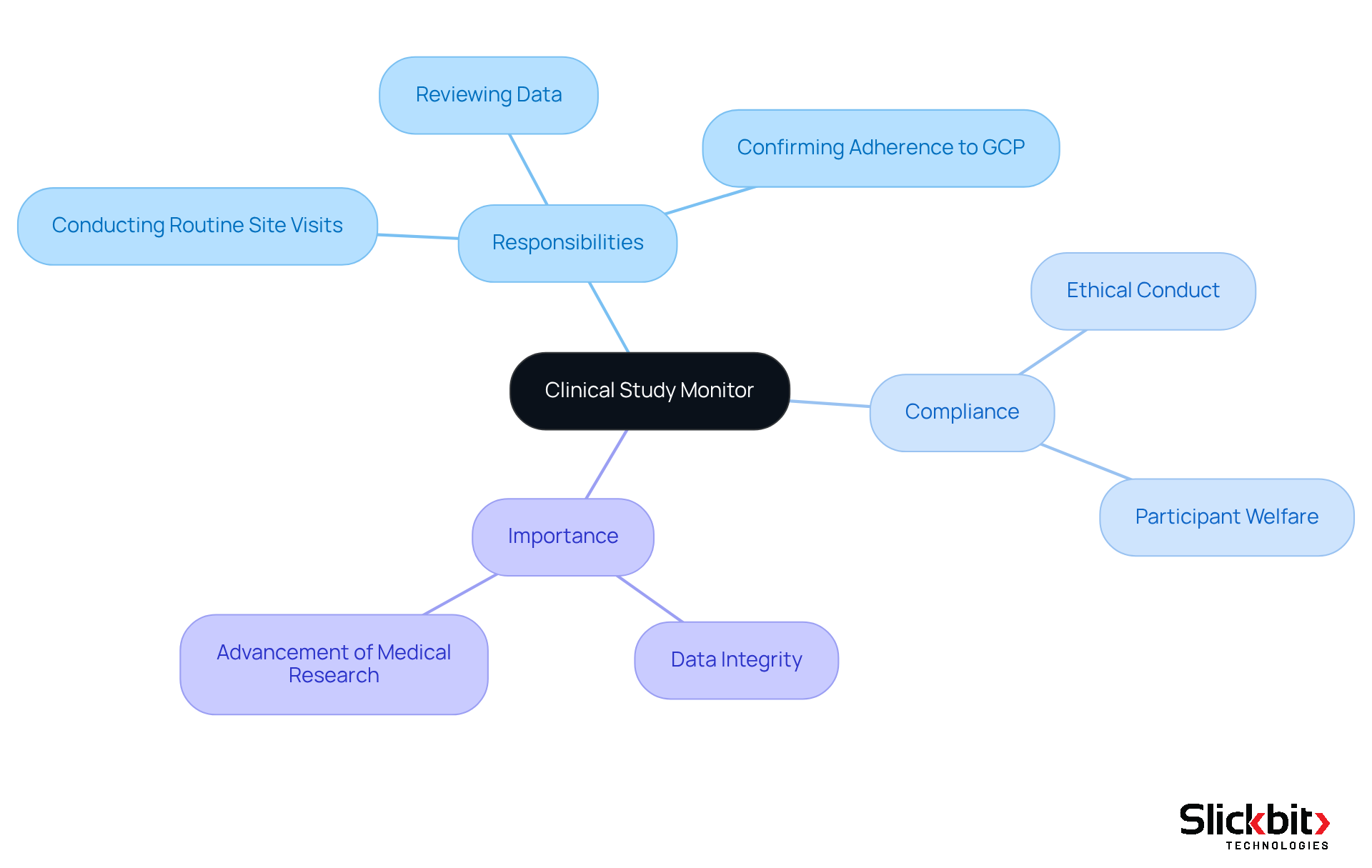
Define Clinical Study Monitor: Role and Importance
A clinical study monitor, often referred to as a Research Associate (CRA), plays a pivotal role in overseeing the execution of clinical studies to ensure compliance with regulatory standards and study protocols. The primary responsibility of a Study Monitor is to ensure that the study is conducted ethically, safeguarding the rights and welfare of participants. This involves:
- Conducting routine site visits
- Reviewing data
- Confirming adherence to Good Clinical Practice (GCP) guidelines
The importance of this position cannot be overstated; the clinical study monitor is essential in maintaining the integrity of medical studies, ensuring that the data collected is both reliable and valid. Consequently, their work is fundamental to the advancement of medical research and the protection of participant rights.
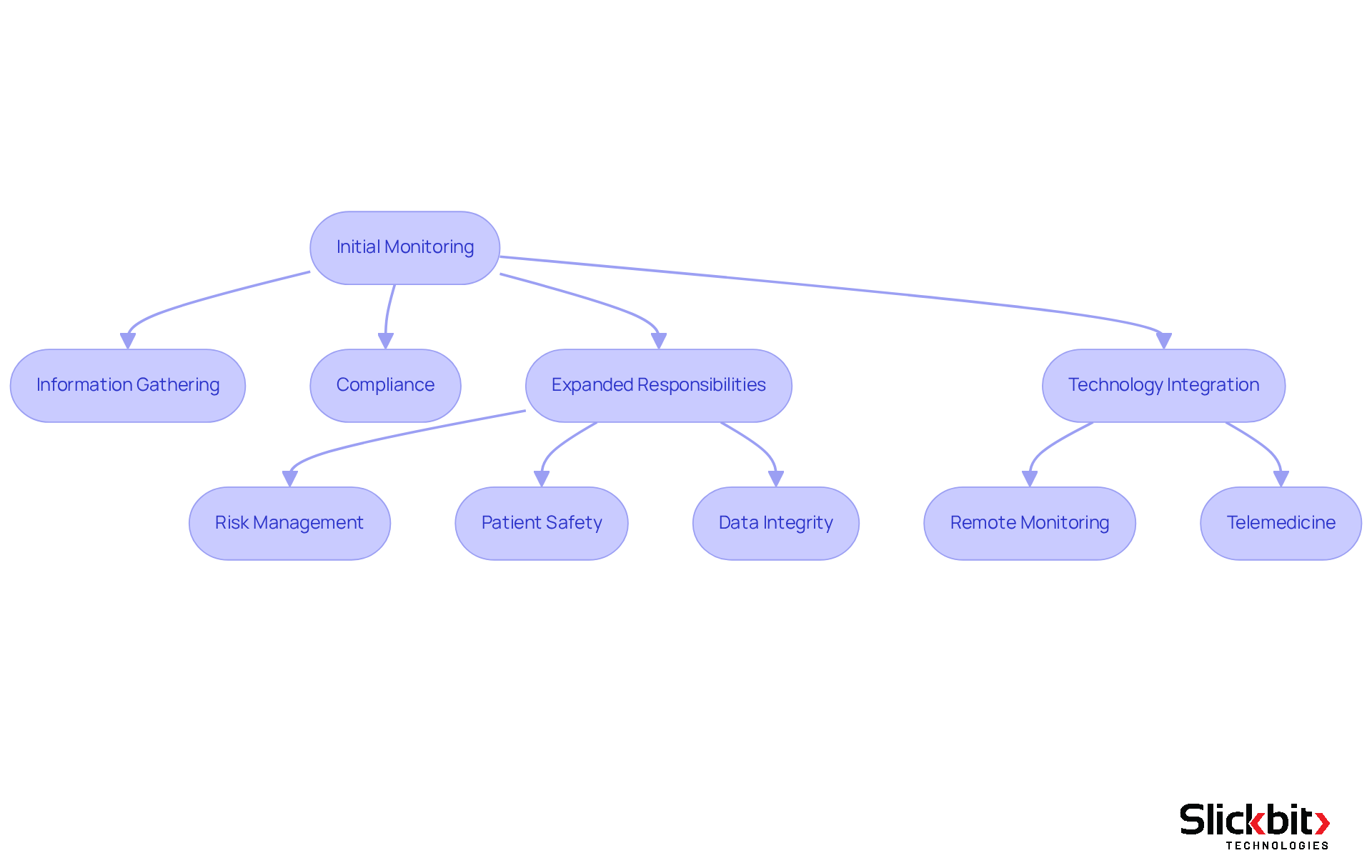
Trace the Evolution of Clinical Study Monitoring
The function of the clinical study monitor has undergone a significant transformation since the early days of clinical research. Initially, monitoring was a straightforward process focused primarily on information gathering and ensuring compliance with regulatory standards. However, as research studies have grown in complexity, the responsibilities of Study Monitors have expanded accordingly. Today, they are entrusted with a broader range of duties, including the responsibilities of a clinical study monitor, which encompass risk management, oversight of patient safety, and the assurance of data integrity throughout the trial process.
Statistics reveal a marked increase in the responsibilities of Study Monitors over recent years. For instance, the average number of tasks assigned to monitors has surged by over 30% in the past decade, reflecting the heightened demands of contemporary clinical research. Furthermore, the average turnover rate for Clinical Research Associates (CRAs) in the U.S. stands at nearly 23%, highlighting the challenges of workforce stability and its implications for monitoring roles. This evolution underscores the critical importance of their role in safeguarding participant welfare and ensuring the quality of research data.
The emergence of technology has revolutionized the practices of clinical study monitoring. Electronic data capture systems have streamlined data collection, while remote monitoring tools facilitate real-time oversight of research sites, reducing the need for frequent on-site visits. These innovations not only enhance the efficiency of the clinical study monitor but also improve the accuracy of monitoring activities. For example, the increasing use of telemedicine for follow-up visits allows monitors to engage with participants without the logistical hurdles of travel. Notably, 70% of the population resides two hours or more from an academic medical center, underscoring the necessity for decentralized trials and remote monitoring tools to enhance patient engagement and recruitment.
Moreover, the integration of advanced analytics and artificial intelligence into monitoring processes has further transformed the role of the clinical study monitor. These technologies enable proactive risk assessment and empower monitors to identify potential issues before they escalate, thereby bolstering patient safety and ensuring compliance with regulatory requirements. As the landscape of medical research continues to evolve, the function of Study Monitors will undoubtedly adapt, driven by the need for greater efficiency, precision, and participant-centered approaches. Additionally, the One Big Beautiful Bill Act introduces heightened compliance demands, which will further shape the responsibilities of Study Monitors in the future.
Detail Responsibilities of Clinical Study Monitors
The role of clinical study monitors is pivotal in the success of clinical studies, as they are tasked with various responsibilities that ensure strict adherence to study protocols and regulatory standards. These professionals conduct site visits to verify compliance, typically every four to six weeks, depending on the complexity of the study and enrollment rates. During these visits, monitors meticulously review and validate data accuracy, a crucial factor considering that protocol deviations can severely impact the reliability of study data and the safety of participants.
Informed consent represents another critical area of oversight; monitors guarantee that participants are fully informed and that consent is obtained in accordance with regulatory requirements. They actively oversee participant safety, addressing any adverse events or protocol deviations that may arise. For example, significant protocol deviations, such as the failure to conduct necessary safety assessments, must be promptly identified and reported to uphold the integrity of the study.
Effective communication is vital in this role. Monitors maintain open lines of communication with the study team, providing ongoing training and support to site staff to enhance compliance and operational efficiency. Experienced Clinical Research Associates (CRAs) emphasize that their role extends beyond mere oversight; they are instrumental in fostering collaboration between sites and sponsors, ensuring that any concerns or disagreements are addressed constructively.
The diverse responsibilities of a clinical study monitor not only support adherence but also enhance the overall quality and dependability of research studies, ultimately improving patient safety and study outcomes. With the emergence of AI technologies, monitors can utilize advanced tools to identify trends in compliance and systemic risks, further bolstering their oversight capabilities. Principal investigators bear ultimate responsibility for the study during regulatory audits, underscoring the importance of adherence to protocols and the timely reporting of deviations. As Robert F. Church, a partner in medical research, states, "Investigators should report to the sponsor all protocol deviations of which they are aware," emphasizing the collaborative nature of this oversight.

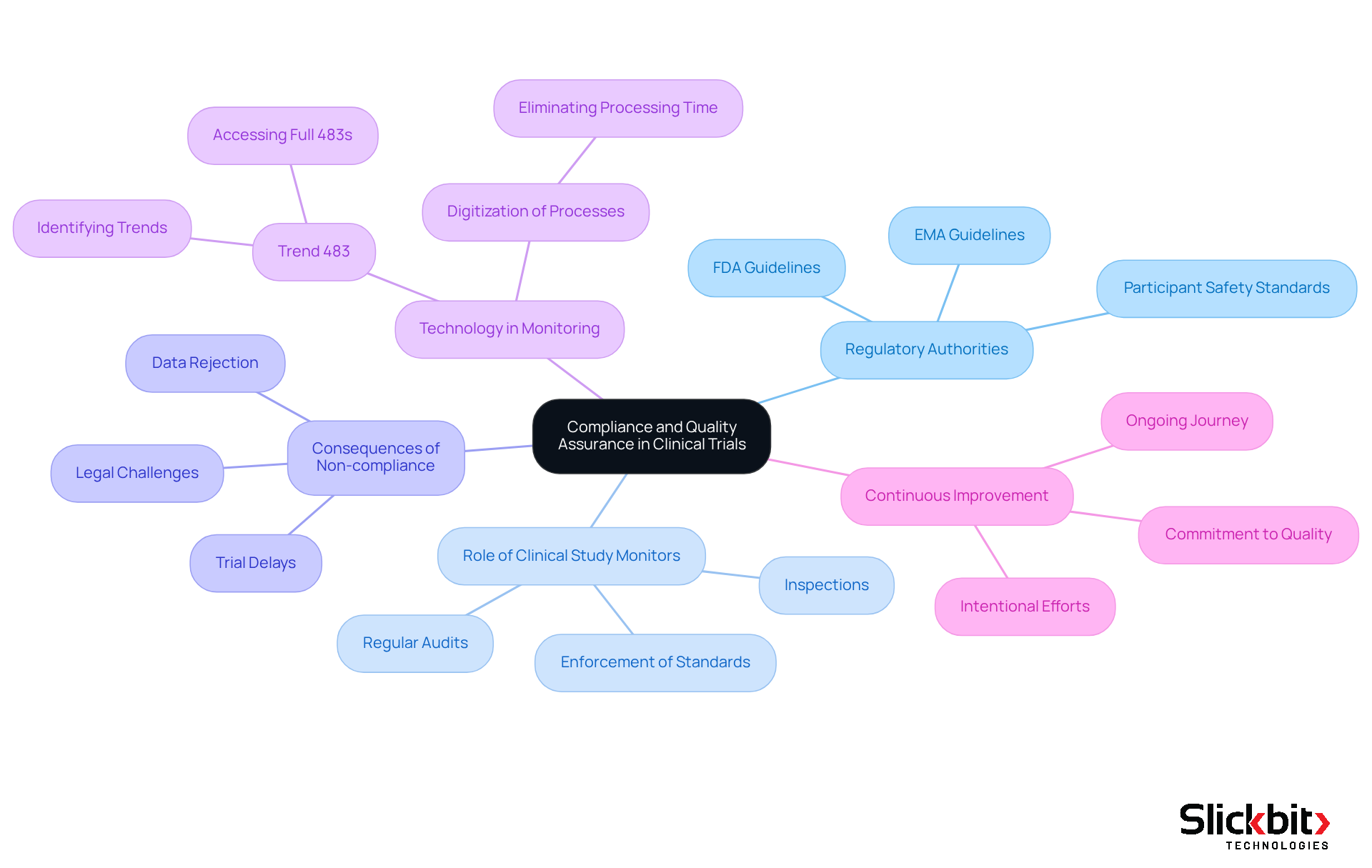
Highlight the Importance of Compliance and Quality Assurance
Adherence and quality control are paramount to the integrity of clinical trials, ensuring ethical conduct and the trustworthiness of the information gathered. Regulatory authorities, including the FDA and EMA, enforce stringent guidelines designed to protect participant safety and uphold the integrity of data.
Within this framework, the role of the clinical study monitor is crucial, as they conduct regular audits and inspections to enforce these standards. Non-compliance can lead to severe repercussions, such as trial delays, data rejection, and potential legal challenges.
Current statistics underscore the necessity for organizations in life sciences to balance the urgency of bringing products to market with the imperative of enhancing overall product and service quality. For example, digitizing the annual review process has demonstrated the ability to eliminate time wasted on processing forms, showcasing the efficiency gains achievable through robust compliance practices.
Furthermore, the implementation of AI technologies like Trend 483 can significantly enhance compliance monitoring by identifying trends in systemic risks and recurring violations from FDA inspections. Trend 483 empowers users to search, filter, and access full 483s for deeper insights, thereby improving the monitoring process.
This commitment to adherence and quality control transcends mere regulatory obligation; it is essential for preserving the credibility of medical research and advancing medical science. As emphasized by industry leaders, achieving quality necessitates intentional efforts and a commitment to continuous improvement, reinforcing that excellence in clinical research is an ongoing journey rather than a one-time achievement.
Conclusion
The role of a clinical study monitor is indispensable in the realm of medical research, serving as a guardian of ethical standards and data integrity throughout clinical trials. By ensuring compliance with regulatory frameworks and study protocols, clinical study monitors uphold the rights and welfare of participants, which is foundational to the credibility of medical advancements.
Throughout this article, key aspects of the clinical study monitor's responsibilities have been explored. From conducting routine site visits and validating data accuracy to fostering effective communication among study teams, these professionals are integral to maintaining the quality and reliability of research outcomes. Furthermore, the evolution of their role, driven by technological advancements and increasing regulatory demands, highlights the growing complexity and importance of their contributions in safeguarding participant safety and enhancing the overall quality of clinical trials.
Ultimately, the significance of clinical study monitoring extends beyond regulatory compliance; it is about fostering trust in the medical research process and ensuring that innovations in healthcare are built on a solid foundation of ethical practice and rigorous data integrity. As the landscape of clinical research continues to evolve, embracing advancements in monitoring practices and technologies will be crucial for achieving excellence in medical studies. Engaging with these developments not only enhances patient safety but also propels the field of medical research forward, making it imperative for stakeholders to prioritize and invest in robust clinical study monitoring practices.
Frequently Asked Questions
What is the role of a Clinical Study Monitor?
A Clinical Study Monitor, often called a Research Associate (CRA), oversees the execution of clinical studies to ensure compliance with regulatory standards and study protocols.
What are the primary responsibilities of a Clinical Study Monitor?
The primary responsibilities include conducting routine site visits, reviewing data, and confirming adherence to Good Clinical Practice (GCP) guidelines.
Why is the role of a Clinical Study Monitor important?
The role is crucial for maintaining the integrity of medical studies, ensuring that the data collected is reliable and valid, and safeguarding the rights and welfare of participants. Their work is fundamental to advancing medical research.




